Gynecological Imaging Using ultraSound
PROJECT ACRONYM
GYNIUS
FUNDED BY
NWO-OTP
PHD CANDIDATE
Frieda van Limbeek (UT) July 2021
Claudia Manzini (UMCU) Spring 2022
Shreya Das (RadboudUMC) Winter 2022
SUPERVISORS
Chris de Korte and Anique Bellos-Grob
COLLABORATION
UMCU, RadboudUMC
CLINICAL BACKGROUND
The puborectalis muscle (PRM) is the pelvic floor muscle, which encircles the rectum, urethra and vagina. It plays a critical role in maintaining continence, providing support to the pelvic organs and allows normal vaginal childbirth. During childbirth the muscle may have to stretch up to 3 times its original length, which can cause trauma to this muscle. This is the main reason that one in four women above the 40 years old suffers from urinary incontinence and one out of six will have a pelvic organ prolapse. This has a substantial negative influence on physical, emotional and social well-being.
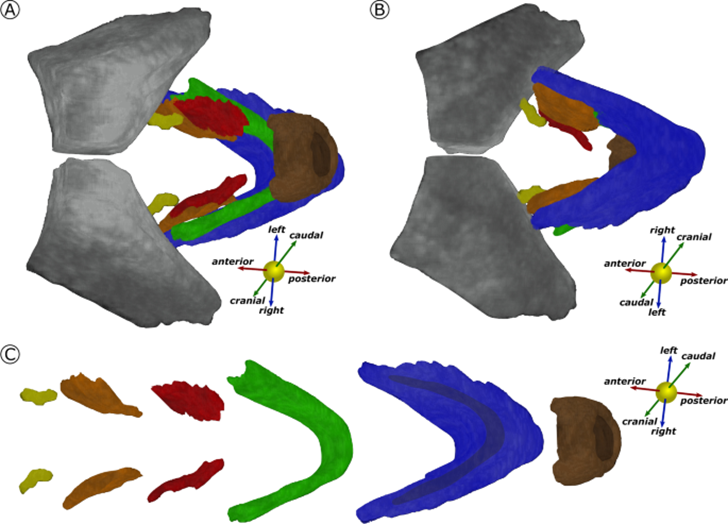
Figure 1 The 3D model showing the segmented structures: The Pubic bone (PB, grey), external sphincter (ES, brown), puboperineal muscle (PPM, red), puboanal muscle (PAM, orange), pubovaginal muscle (PVM, yellow), puborectal muscle (PRM, green) and iliococcygeal muscle (ICM, blue). A shows the view from caudal to cranial; B shows the view from cranial to caudal. In C, the model is disassembled to appreciate the single structures separately.
OBJECTIVE
Obtaining functional information about the PRM is crucial in understanding mechanisms associated with pelvic floor (dys)function, and in providing diagnostic and therapeutic important information. Since the PRM is located deep inside the pelvis obtaining direct functional information, like EMG or direct muscle force recordings, is not feasible.
In this project we aim develop functional imaging methods based on deformation (strain) quantification as derived from 3D and 4D ultrasound recordings as already applied in cardiology. Although the PRM can be visualized with 3D and 4D transperineal ultrasound, current post-processing analysis tools only allow us to obtain indirect functional information in a 2-D reconstruction. We are dedicated to unveil the 3D anatomical and functional information about the PRM and to integrate these findings into a reliable clinical workflow. In order to do so we will address the following topics:
- Development of Automatic Segmentation and Static Tissue Characterization software. This will allow us to reconstruct accurate 3-D models of the PRM and identify and study structural integrity.
- Development of Functional Measurements. Strain and tissue elastography measurements will be incorporated to improve diagnosis of pelvic floor (dys)function and guide clinical practice. (MUSIC, Radboud UMC).
- Clinical Relevance and Validation. The developments under 1 and 2 will be continuously tested on clinical datasets of the target populations during the study period. This will allow direct developmental feedback in general and for specific clinical indications summarized under. (Vrouw en Baby, UMC Utrecht).
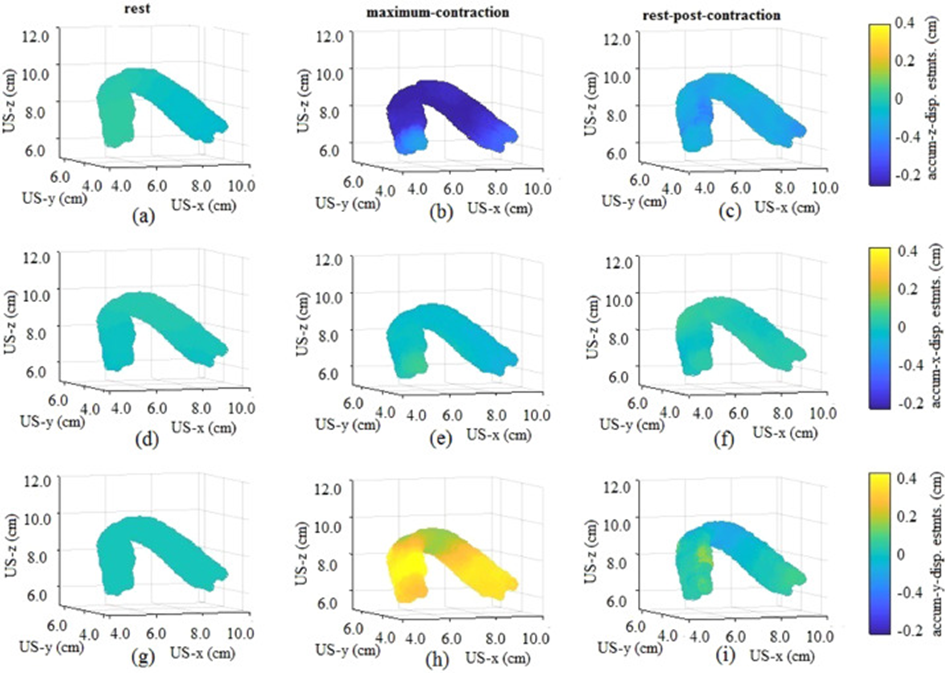
Figure 2 Accumulated displacement estimates at three time points during the rest-contraction-rest sequence of volunteer 1. (a-c) Accumulated z-direction displacement estimates. (d-f) Accumulated x-direction displacement estimates. (g-i) Accumulated y-direction displacement estimates).
PROJECT DETAILS
The pelvic floors of more than 450 women are scanned by means of transperineal ultrasound. Automatic detection and segmentation of one specific muscle (puborectalis) is realized. Successful strain analyses by means of dedicated software is possible, but the software needs improvement to allow for clinical validation.
We are looking for students on the following research projects:
- Optimizing the ultrasound strain software (shorten analyses time). In that way the tool can be used in clinical validation studies
- Translating the software tool from the puborectalis muscle to the rectal sphincter. Same clinical questions on reliability and proper functional assessment are in play.
PUBLICATIONS
- Van den Noort F, Manzini C, van der Vaart CH, van Limbeek MAJ, Slump CH, Grob ATM. Automatic identification and segmentation of the slice of minimal hiatal dimensions in a transperineal ultrasound volume. Ultrasound Obstet Gynecol 2021.
- Manzini C, van der Vaart CH, van den Noort F, Grob ATM, Withagen MIJ. Pessary fitting for pelvic organ prolapse: parameters associated with specific reasons for failure. Int Urogynecol J 2021.
- Manzini C, Grob ATM, van den Noort F, Withagen MIJ, van der Vaart CH. Transperineal ultrasound to estimate the appropriate ring pessary size for women with pelvic organ prolapse. Int Urogynecol J 2021.
- Manzini C, van den Noort F, Grob ATM, Withagen MIJ, Slump CH, van der Vaart CH. Appearance of the levator ani muscle subdivisions on 3D transperineal ultrasound. Insights into Imaging 2021.
- Manzini C, Morsinkhof LM, van der Vaart CH, Withagen MIJ, Grob ATM. Parameters associated with unsuccessful pessary fitting for pelvic organ prolapse up to three months follow-up: a systematic review and meta-analysis. Int Urogynecol J 2021.
- Manzini C, van den Noort F, Grob ATM, Withagen MIJ, van der Vaart CH. The effect of pessary treatment on puborectalis muscle function. Int Urogynecol J 2021.
