Development of a real-time visualization strategy in Selective Internal Radiotherapy using Dynamic Contrast Enhanced Ultrasound
PhD candidate:
Jan van der Hoek
Supervisors:
dr. E. Groot Jebbink, prof. dr.-ing J. Arens, prof. dr. S. Manohar
Collaboration:
This project is a collaboration between the University of Twente, Ghent University and Radboudumc Nijmegen.
Clinical background
Liver cancer is one of the leading cancer mortalities worldwide. It is expected that by 2025 more than one million people per year will contract liver cancer globally [1]. Surgical resection of the liver tumor is preferable as it increases the survival rate and life expectancy, however, this is not always possible. At this unresectable stage, a life enhancing treatment called Selective Internal Radiotherapy (SIRT), also referred to as radioembolization, is often used. In hepatic radioembolization, radioactive particles are injected into one of the hepatic arteries by a microcatheter (see Figure 1). The radioactive particles travel downstream towards the arterioles, where they embolize and irradiate liver malignancies over time.
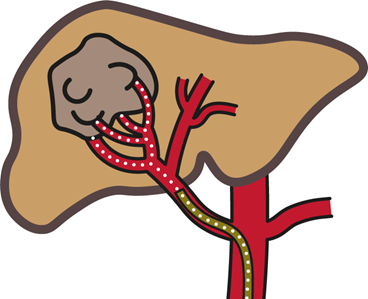
Figure 1: Schematic overview of the SIRT procedure. The microspheres (white) are injected through a catheter (yellow).
The radioactive particles are microspheres containing Yttrium-90 or more recently also Holmium-166 [2]. Microspheres containing Holmium-166 have advantages over Yttrium-90 microspheres regarding imaging possibilities, as the paramagnetic effects and emitted γ-radiation of Holmium-166 make it suitable for MRI and SPECT scanning. While Holmium-166 microspheres already allow for better imaging and a wider variety of imaging modalities like SPECT and MRI, there is still a clear unmet need for (real-time) visualization in patient specific situations [3].
Objective
To overcome the challenges regarding visualization of the procedure, a change to the radioembolization protocol is proposed. To predict microsphere behaviour, contrast microbubbles can be injected to act as microsphere precursors. Visualization and quantification of these microbubbles can then be realized by using dynamic contrast enhanced ultrasound (DCE-US), thus enabling visualization during the procedure [4]. The first objective is to investigate the extent to which the microbubbles can predict microsphere behavior. Using these results, a real-time visualization strategy will be developed and tested in several controllable environments. These results will incentivize a change in radioembolization protocol that gives more insight into the procedure and eventually improve treatment outcomes.
Project details
The development of the visualization strategy for radioembolization will go through several stages to prove clinical feasibility. These include in-vitro tests in simple and more complex patient specific models, but also in-vivo experiments with pig livers and human livers.
Currently, the transport behavior of microspheres and microbubbles are compared in-vitro. The downstream distributions of both particle types are compared in an arterial phantom that represents the right hepatic artery, which is investigated both experimentally and numerically by using CFD. The main aim is to obtain clear results regarding the ability of microbubbles to act as Holmium-166 microsphere precursors, which will provide an indication of the feasibility of developing the real-time visualization strategy.
With clinical feasibility as one of the main topics, an ex-vivo pig liver setup is used to serve as a proof-of-concept for the strategy. For this reason, a perfusion system is designed that is suitable for multiple imaging modalities. Currently, organ viability is investigated to test the designed setup in a clinical environment by using MR imaging.
Publications
[-]
References
1. Cyriac A. Philips , Sasidharan Rajesh , Dinu C. Nair , Rizwan Ahamed , Jinsha K. Abduljaleel , Philip Augustine, Hepatocellular Carcinoma in 2021: An Exhaustive Update, Cureus, 2021.
2. C. van Roekel, R. Bastiaannet, M. L. Smits, R. C. Bruijnen, A. J. Braat, H. W. de Jong, S. G. Elias, and M. G. Lam, “Dose–Effect Relationships of 166Ho Radioembolization in Colorectal Cancer,” Journal of Nuclear Medicine, vol. 62, no. 2, 2 2021.
3. Nijsen JF, Seppenwoolde J-H, Havenith T, Bos C, Bakker CJ, van het Schip AD. Liver tumors: MR imaging of radioactive holmium microspheres—phantom and rabbit study. Radiology. 2004;231(2):491-499.
4. Jakobsen JÅ, Oyen R, Thomsen HS, Morcos SK, Members of Contrast Media Safety Committee of European Society of Urogenital R. Safety of ultrasound contrast agents. European Radiology. 2005;15(5):941-945.
