Ambition
In the coming years, due to the aging of the population and the low availability of donor organs there will be urgent need for bioengineering solutions to assist, mimic or replace failing patient organs. This chair has the ambition, to take-on the challenge of helping the patients by developing (bio) artificial organs. These organs would be:
- Artificial: based on new biomaterials and novel designs, to assist or mimic a patient organ. Typical examples here are: (i) new generation of artificial kidney devices for better and more continuous patient treatment – including portable kidney devices (ii) new artificial liver devices for blood detoxification using novel sorbents.
- Bioartificial: combining biomaterials and biological cells to fully replace failing patient organs. Typical examples here are: (i) bioartificial kidney devices, combining biomaterials and kidney epithelial cells for improved blood detoxification (ii) bioartificial pancreas devices, combining encapsulation of pancreatic cells for treatment of diabetes (iii) development of a bioartificial lungs for studying lung regeneration.
In this field of research, the challenges (scientific and technological) are big. There is need for new biomaterials, need for better understanding and tailoring of the biomaterial – cell / tissue interaction, better immune protection and mass transfer, as well as, development of new concepts and designs. The complexity increases from artificial to bioartificial organs, and the engineering and regulatory demands increase further if these organs would be extracorporeal or implantable.
The chair of (bio) artificial organs addresses several of these challenges by developing an innovative research program, which combines a wide spectrum of disciplines: from molecule to organ.
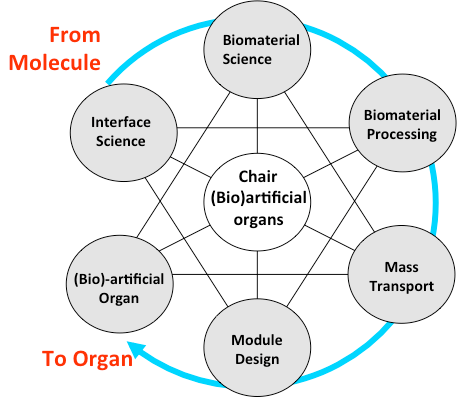
Illustration of the disciplines within the chair of (Bio)artificial organs.
For more information, please contact:
Prof. Dr. Dimitrios Stamatialis
d.stamatialis@utwente.nl
ZH 242, Tel: +31 (0)534894675 or +31 (0)534892968
